The Conrad N. Hilton Foundation’s Early Childhood Development – U.S., Foster Youth, Homelessness and Opportunity Youth initiatives are expanding place-based approaches to mental health services.

Mental health care and wellness should be accessible for everyone. In the United States, it is often those who need mental health services the most who face systemic barriers to treatment. It is crucial to adopt a comprehensive approach to services that includes reducing stigma, increasing access to mental health services, promoting equity, and mending a fragmented system of care.
An equitable mental health care system considers an individual’s location, background, identities, lived experience and other unique factors that can act as barriers to accessing quality mental health services. For example, rural areas often face a shortage of mental health care providers. Equitable solutions for remote geographies would include alternative care options such as telehealth services, mobile clinics and integration with primary care facilities.
To achieve this goal, we are exploring community- and place-based programs for mental health care across four of our program initiatives: Early Childhood Development – U.S., Foster Youth, Homelessness and Opportunity Youth. We understand that supporting emotional and mental well-being is essential to improving outcomes for parents and children, youth entering adulthood, and individuals seeking permanent housing.

The April Issue of Health Affairs, “Perinatal Mental Health and Well-Being,” provides a broader understanding of maternal mental health challenges and the solutions. The issue focuses on research, analyses and commentaries about various aspects of perinatal mental health, such as addressing health disparities, making services more accessible and equitable, improving access to care, and tailoring solutions, including innovative approaches for Tribal communities.
1 in 5 women experience mental health or substance use disorders during the perinatal period from pregnancy until one year after birth. A lack of screening, inaccessible maternal care options, and shame around mental illness prevent mothers from seeking help. About 75% of people with perinatal mental health issues never seek treatment, and the ratio of those not seeking treatment is even higher for Black, Latinx and Tribal communities.
Families, especially young children, feel the impact of maternal trauma. When mothers stress-regulation genes are activated they are passed down to the child and encoded in their DNA, leading to an “intergenerational transmission” of trauma during the perinatal period. We partner with communities to embrace an intergenerational approach to building wellness and well-being.
Collaborative Efforts to Improve Maternal Mental Health from L.A. County Providers
We’ve partnered with clinical and community-based organizations across Los Angeles County to test various approaches to support parent’s and children’s health. A holistic approach to wellness for families provides different mental health care options, with both clinical and non-clinical approaches to meet the unique mental, physical and emotional needs of parents and caregivers and their children.
Programs include community-based doula services, perinatal community health workers, birth centers, breast-feeding and lactation peer counselors, and group prenatal care. Addressing disparities in access to trauma-informed care as well as education and engagement on the community- and institutional-level are all crucial to provide holistic maternity care. This approach considers the lived experiences during the perinatal period, including acknowledging the caregivers’ childhood traumas and inequities.
Our partners include African American Infant and Maternal Mortality (AAIMM), Charles Drew University – Black Maternal Health Center of Excellence, MLK Community Health, Maternal Mental Health Now, Project Joy and Westside infant family network.
Young people are leading the way to make mental health care accessible, integrated and high-quality for youth in and transitioning out of foster care. Approximately 80% of children in foster care report having significant mental health needs while facing unique adversity and trauma. In California, new benefits, commitments and policy reforms, guided by the experiences of youth in foster care, are poised to transform the mental health services system from medically stigmatizing to comprehensive, trauma-informed and community-based.
Breaking down barriers to care
Children Now teamed up with youth in the foster care system to expand access to Specialty Mental Health Services (SMHS) without a formal diagnosis in California’s Medicaid program, Medi-Cal, through CalAIM (California Advancing and Innovating Medi-Cal), a state initiative to transform Medi-Cal to create a more coordinated, person-centered and equitable health system. Through feedback on CalAIM proposals, foster youth called out the stigma of diagnoses, arguing they were often inaccurate and a barrier to access critical mental health support.
This powerful advocacy led to a significant victory: AB 133. Effective January 1, 2022, children and youth with child welfare involvement or experiences of trauma became categorically eligible for SMHS, allowing them to access services as needed. Today, Children Now continues to monitor implementation, requesting state-wide data to ensure children and youth have reliable access to SMHS.
Evidence-backed decision-making
This pivotal moment for youth mental health care is demonstrated by the comprehensive state-commissioned report released last year by California’s Department of Health and Human Services and guided by California Children Trust’s Youth Advisory Board, community-based organizations, youth and caregivers. The Youth At The Center (YAC) report offers 12 recommendations to improve mental health services in California.
We also support California Children’s Trust’s work to provide comprehensive wraparound support for all youth in the foster care system. They recently released the final paper of a four-part series that makes the case for wraparound mental health services for youth in foster care, identifying opportunities for implementation at the policy and community-level.
Wrapround services acknowledge that some young people need access to services beyond talk therapy and medication to improve their mental health and well-being. We’re investing in programs that offer alternative mental health services across the U.S., including Creative Wellbeing in Los Angeles, Foster Care Unplugged and Soul Care project, both in New York City.

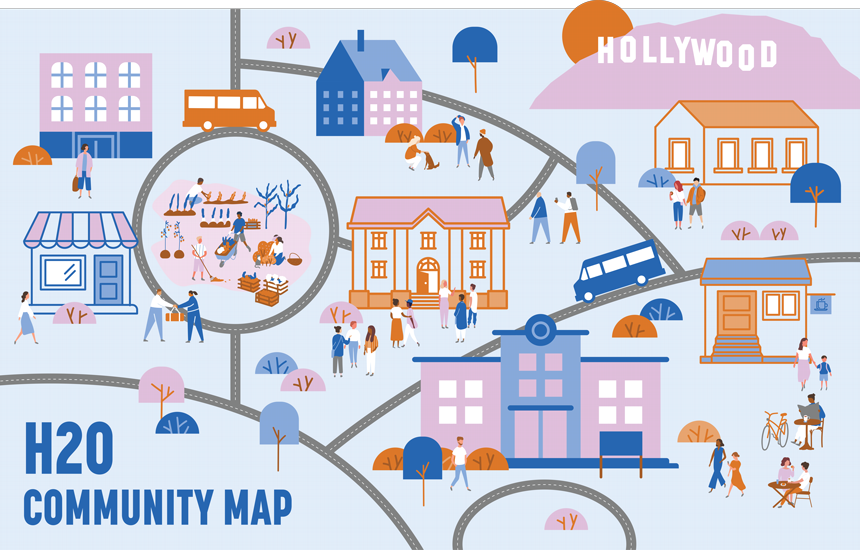
In Hollywood, CA, the Los Angeles County Department of Mental Health is piloting a new comprehensive community care model addressing isolation through place-based mental health services. The plan is called Hollywood 2.0, and it aims to create an ecosystem of care with the help of residents and 51 organizations in the Hollywood community.
For those diagnosed with severe mental illness and coping with substance use disorder, experiencing unsheltered homelessness is especially traumatizing and isolating. External stressors exacerbate mental health challenges, and a visit to the emergency room can heighten fear and anxiety rather than treat it.
With Hollywood 2.0, each service is designed to meet the needs of the individual, from respite and recovery centers, board and care, interim housing, mental health cooperative clinics, employment and community events. While hospitals play a vital role in emergencies, place-based services offer a more comprehensive and supportive approach to long-term mental health needs, especially for those experiencing homelessness.
We support several organizations implementing Hollywood 2.0, including the broad-based coalition Hollywood 4WRD, the historic Center in Hollywood and the new Fountain House on Sunset Blvd.
Here’s how they contribute to a community-based mental health model in Los Angeles:
Accessibility:
The Foundation began supporting The Center in Hollywood back in 2014 to help them address isolation and end homelessness through community. Today, their model embraces radical hospitality, offering a welcoming and familiar space for those experiencing homelessness and mental health challenges to find community and feel accepted.
Holistic Care:
The Center’s wrap-around supports tailor solutions so every person can decide how they want to practice wellness. From community discussion groups, music and art sessions, the Center provides holistic services to recovery by investing in each person’s sense of identity as well as their physical health. Through a partnership with Saban Community Health Clinic, they also offer onsite clinicians, harnessing the welcoming nature of the Center to also encourage their visitors to check in with their clinical care provider.
Continuity:
Fountain House’s clubhouse model is recognized worldwide for its recognition of community as a form of therapy. The model emphasizes that social connection is essential to recovery. Fountain House is also the 2014 Hilton Humanitarian Prize Laureate. Clubhouses provide a range of services, including employment, education, housing, meals and support for building relationships. Members work with social practitioners to create goals, build their confidence, and find purpose and belonging. With consistent support, members are offered a sustainable path to recovery that is unlike traditional mental health services because it is tailored to their specific needs.
Community Integration:
Hollywood 2.0 is an innovative program that provides mental health services integrated into the community, aiming to ensure no one experiencing homelessness or a mental health crisis falls through the cracks. The Hollywood 2.0 map (pictured below) illustrates the model: an interim shelter would be a few doors down from a clubhouse, where members can access employment services before heading to The Center for art therapy sessions. The goal is to foster stability and support for long-term recovery and placement in permanent housing.
Every young person needs community based and individualized care to support their mental health and well-being. However, despite this, some young people have found that current systems of care may not meet their unique needs. Opportunity youth, young people between the ages of 16-24 who are seeking employment and education, face particular barriers to receiving this kind of culturally competent and individualized care. A lack of mental health supports and strong ties to the community can make it more difficult for young people to reconnect to education, training and employment.
Opportunity youth deserve access to strong mental health services to support them as they pursue education and skills training to secure meaningful work. We are supporting a new peer-to-peer mental health model integrated with workforce development programs to ensure young people have the systemic support they need to succeed.
Peer-to-peer mental health models help young people build a network of health supports in their community by connecting youth to trained peer mental health specialists who can address basic needs, aspirations and fears. Since many young people deeply trust and prefer to speak with others like them, access to these community-based models meet young people where they are at, helping them build roots within their community, and can ease the way if higher-touch clinical care might be needed.
Recognizing that peer-to-peer mental health supports could help young workers seeking jobs, the Economic and Workforce Development Department took advantage of recent changes to the state’s Medicaid program to adopt a new model of providing community based care across its 14 YouthSource Centers. The program gives young people access to mental health support in community-based settings from their trusted peers, as they engage in workforce and skills training that leads to employment. The program also builds a pathway for youth to seek careers in behavioral health, as the certified youth peer specialists who complete the program will be eligible for hire as Medicaid-reimbursable providers through L.A. County’s Department of Mental Health.